Hepatitis C and Liver Damage

Hepatitis C and Liver Damage
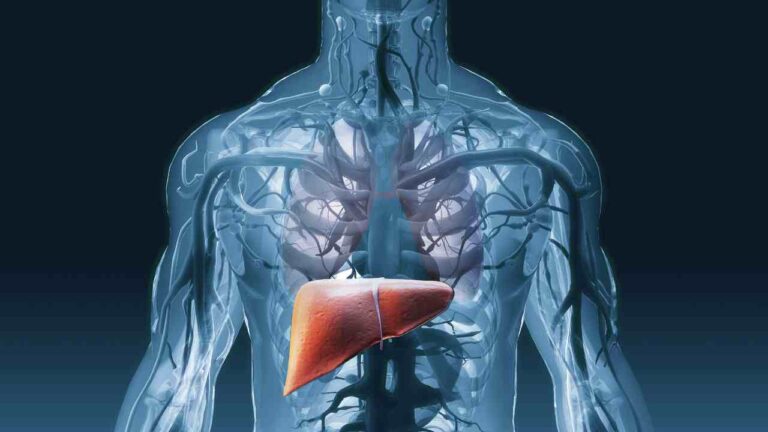
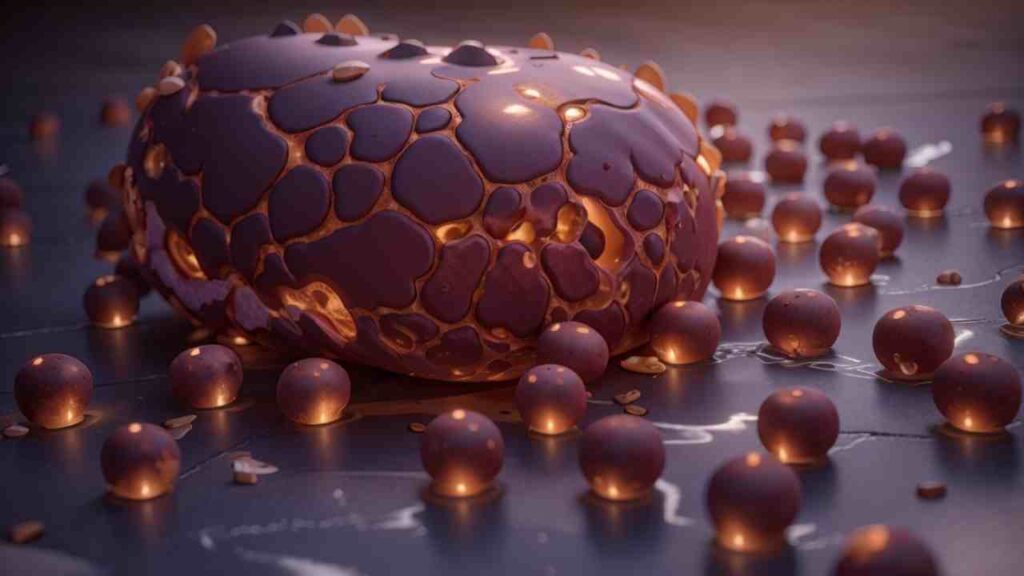
Hepatitis C is a viral infection that can lead to liver damage. The virus attacks and inflames the liver, causing it to become swollen and dysfunctional. This damage occurs gradually over time, as the virus replicates and spreads throughout the liver cells. If left untreated, hepatitis C can progress to more severe forms of liver damage, such as cirrhosis or liver cancer. It is important to recognize the symptoms of liver damage, which may include fatigue, jaundice, and abdominal pain, as early diagnosis and treatment can help prevent further complications. Furthermore, managing liver damage through lifestyle changes and medication can also improve outcomes for individuals with hepatitis C. Overall, understanding the mechanisms and progression of liver damage is crucial in order to effectively diagnose, treat, and prevent the complications associated with hepatitis C.
2. Hepatitis C and Liver Damage
Mechanisms of Liver Damage
Damage to the liver resulting from hepatitis C evolves over time and can lead to severe complications. The damaging process often transpires in stages, commencing with liver inflammation. As the disease advances, fibrosis can set in, where scar tissue begins to replace healthy liver cells. This unchecked damage can escalate to cirrhosis, when the liver is heavily scarred and its function is severely impaired. The chain of liver deterioration can also result in hepatocellular carcinoma — a form of liver cancer. Recognizing early signs of liver damage and pursuing early diagnosis and treatment can forestall further complications.
Progression of Liver Damage
Liver deterioration is a common fallout of a hepatitis C infection. The signs of liver deterioration can fluctuate from one individual to another and may include throttling fatigue, jaundice, abdominal discomfort, and leg or ankle swelling. As the liver’s condition worsens, more fearsome symptoms can emerge, such as fluid buildup in the abdomen, disorientation, and blood clotting disorders. It’s worth noting that some hepatitis C victims might not display any signs of liver damage until the disease is in advanced stages. If ignored, liver damage can result in complications such as cirrhosis and liver cancer. Timely recognition, diagnosis, and treatment of hepatitis C are therefore instrumental in avoiding further liver damage and enhancing prognostic outcomes.
Symptoms of Liver Damage
Liver deterioration is a typical complication of hepatitis C. As the virus colonizes the liver, it incites inflammation, leading to a gradual obliteration of liver cells. This deterioration can lead to more severe conditions like fibrosis and cirrhosis, or even liver cancer. During fibrosis, liver tissue becomes scarred, compromising its function. Cirrhosis represents fibrosis’s advanced stage, where the liver is heavily damaged, losing its ability to perform crucial tasks. Both fibrosis and cirrhosis can lead to a range of complications, including portal hypertension—an increased pressure in liver blood vessels, potentially causing dire complications like hemorrhaging or fluid-filled sac development in the abdomen. Hepatocellular carcinoma, a possible complication of long-term hepatitis C infection and liver damage is also of significant concern. Prompt diagnosis, treatment, and management of liver deterioration are fundamental in forestalling these complications and ameliorating the general outcomes for hepatitis C patients.
Complications of Liver Damage
A sustained onslaught of hepatitis C on the liver often results in significant organ damage. It primarily targets the liver cells, causing inflammation and consequential injury, as well as releasing harmful chemicals into the body. Chronic infection can further provoke an immune system offensive against the liver cells. Long drawn out bouts of inflammation and immune response, if left unchecked, can culminate in liver fibrosis: the proliferation of scar tissue. If this fibrosis isn’t treated, it can progress into cirrhosis, where the liver incurs severe functional impairment due to extensive damage. In short, understanding the complex damage mechanisms induced by Hepatitis C is pivotal for the effective diagnosis and treatment of the disease.
Diagnosis and Treatment
Testing for Hepatitis C
Testing for Hepatitis C is deemed essential to identifying the infection and evaluating the ensuing liver damage. Two major types of tests are conducted: antibody tests and nucleic acid tests (NAT). Antibody tests assess whether the body has reacted to the virus by generating antibodies, whereas NATs search for the presence of the virus in the blood. A NAT is used to confirm active infection if the antibody test comes back positive. Supplementary tests could be conducted to ascertain the degree of liver damage, such as liver functional tests or imaging studies. The key role of testing is to detect Hepatitis C promptly, hence trigger treatments that may slow down liver damage progress.
Stages of Hepatitis C
Over time, Hepatitis C can evolve through various phases, each influencing the liver differently. Hepatitis C’s early stage is frequently silent with no evident symptoms, yet, the virus is actively harming the liver at this point. Persistent infections can escalate into liver inflammation and scarring, or what’s termed as fibrosis**. If left untreated, fibrosis can transition into severe stages like cirrhosis, during which the liver accrues significant scar tissue inhibiting its normal operation**. Therefore, it’s pivotal to identify hepatitis C at an early juncture and pursue fitting treatments to deter hepatic deterioration.
Treatment Options
Treatments for Hepatitis C and its impact on the liver strive to suppress or halt the progression of liver damage and avert complications. The usual therapy for chronic hepatitis C comprises a mix of antiviral drugs referred to as direct-acting antivirals (DAAs). By targeting the hepatitis C virus, these medications obstruct its multiplication within the body. DAAs have exhibited high recovery rates and are typically tolerated well. Lifestyle modifications go hand in hand with drug treatment, and they play a significant role in managing the hepatic impairment induced by hepatitis C. Such changes might encompass abstaining from alcohol and certain medications that could inflict supplemental damage to the liver, adhering to a salubrious diet, engaging in regular physical activity, and vaccination against other hepatic diseases such as hepatitis A and B. For a few individuals with critical liver damage, further therapies like liver transplant may be necessitated. However, it’s important to state that due to newer treatments, not all hepatitis C sufferers with related liver damage will need a transplant. With early detection and appropriate treatment, many individuals can achieve a sustained virologic response — meaning they have undetectable levels of the virus in their blood — and thus reduce the risk of further liver damage and complications.
Bibliography
- Sivakrishnan, S., & Pharm, M. (2019). Liver disease overview. World Journal of Pharmacy and Pharmaceutical Sciences, 8(1), 1385-1395. (https://www.researchgate.net/profile/Siva-Krishnan-6/publication/331816198_LIVER_DISEASES-AN_OVERVIEW/links/5ca086daa6fdccd46045e7f4/LIVER-DISEASES-AN-OVERVIEW.pdf)
- Reungoat, E., Grigorov, B., Zoulim, F., & Pécheur, E. I. (2021). Molecular crosstalk between the hepatitis C virus and the extracellular matrix in liver fibrogenesis and early carcinogenesis. Cancers. (https://www.mdpi.com/2072-6694/13/9/2270/pdf)
- Friedman, S. L. (2022). Regression of Fibrosis Following Hepatitis C Eradication. Gastroenterology & Hepatology. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9666799/)
- Roberts, L. R. (2019). Current status of the GALAD and BALAD biomarker models for hepatocellular carcinoma. Gastroenterology & hepatology. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6935027/)
- Jones, A. T., Moreno-Walton, L., Sossamon, S. D., Tahmeena, F., Tran, T., Briones, C., … & Kissinger, P. J. (2023). Delays in fibrosis staging reduce the likelihood of achieving hepatitis C treatment and cure. Infectious Diseases, 55(5), 309-315. (https://www.tandfonline.com/doi/abs/10.1080/23744235.2023.2178670)
- Goodman, S., Zahn, M., Bruckner, T., Boden-Albala, B., & Lakon, C. M. (2021). Measuring hazards of undetectable viral load among hepatitis C antibody positive residents of a large Southern California county. Health services research and managerial epidemiology, 8, 23333928211066181. (https://journals.sagepub.com/doi/full/10.1177/23333928211066181)
- Gobran, S. T., Ancuta, P., & Shoukry, N. H. (2021). A tale of two viruses: immunological insights into HCV/HIV coinfection. Frontiers in Immunology. (https://www.frontiersin.org/articles/10.3389/fimmu.2021.726419/full)
- Chaudhari, R., Fouda, S., Sainu, A., & Pappachan, J. M. (2021). Metabolic complications of hepatitis C virus infection. World journal of gastroenterology, 27(13), 1267. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8015302/)
- Tanwar, S., Rhodes, F., Srivastava, A., Trembling, P. M., & Rosenberg, W. M. (2020). Inflammation and fibrosis in chronic liver diseases including non-alcoholic fatty liver disease and hepatitis C. World journal of gastroenterology, 26(2), 109. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6962431/)
- Shipley, L. C., Axley, P. D., & Singal, A. K. (2019). Liver fibrosis: a clinical update. Hepatology. (https://www.emjreviews.com/wp-content/uploads/2019/05/Liver-Fibrosis-A-Clinical-Update.pdf)
- Luna-Cuadros, M. A., Chen, H. W., Hanif, H., Ali, M. J., Khan, M. M., & Lau, D. T. Y. (2022). Risk of hepatocellular carcinoma after hepatitis C virus cure. World Journal of Gastroenterology, 28(1), 96. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8793019/)