Hepatitis After Pregnancy: Risks, Monitoring, and Treatment Options

Hepatitis After Pregnancy: Risks, Monitoring, and Treatment Options
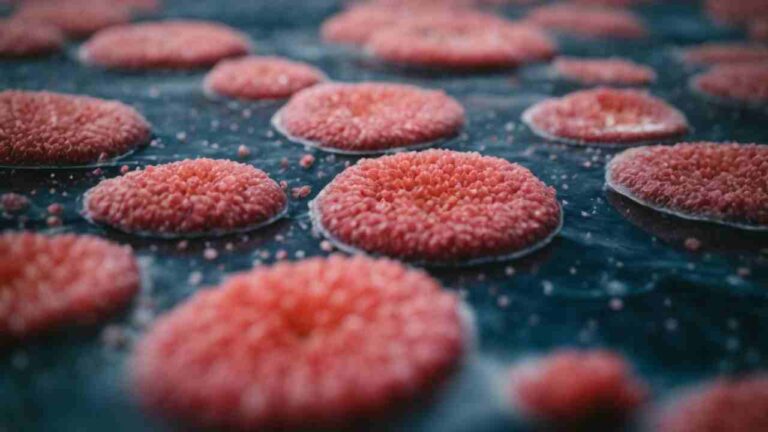
The occurrence of hepatitis after pregnancy, typically diagnosed through elevated alanine aminotransferase (ALT) levels within the first 12 weeks postpartum, presents an intriguing intersection of immunology and maternal health. This condition, often self-limiting, suggests significant underlying immune system adjustments as the body shifts from pregnancy. While the precise mechanisms remain partially understood, the role of hormonal shifts and their impact on inflammatory responses is undeniable. As researchers continue to untangle the complex web of hormonal, immune, and possibly genetic factors involved, the implications for improving postpartum care and developing targeted interventions become increasingly consequential. What could the future hold for understanding and treating postpartum hepatitis, and how might this reshape approaches to maternal health care?
Understanding Postpartum Hepatitis
Postpartum hepatitis, characterized by elevated ALT levels following delivery, typically manifests within the first 12 weeks postpartum and is generally self-limited. This condition underscores the intricate balance of maternal recovery, where liver function plays an important role. The hormonal influence during and after pregnancy can modulate the immune system, potentially leading to an inflammatory response that impacts liver health. Understanding these dynamics is essential for managing and supporting postpartum women effectively. The liver’s ability to recover, influenced by these hormonal and immune changes, usually allows for the resolution of hepatitis without long-term consequences, highlighting the resilience and adaptive capabilities of the maternal body during the postpartum period.
Immune Changes and Hepatitis
Understanding the immune changes during the postpartum period is key to comprehending the mechanisms behind hepatitis development after pregnancy. Post-delivery, the maternal immune system shifts from a pregnancy-adapted state characterized by increased immune tolerance and modulation. This change impacts liver health immensely. Pregnancy hormones, which modulate T cell regulation and suppress certain immune responses to protect the fetus, decline, altering the immune landscape. This alteration can exacerbate an inflammatory response, potentially triggering hepatitis, especially in the presence of HBV infection. NK cell function, important in managing viral infections, also adjusts postpartum. Additionally, liver enzymes, which are often elevated during hepatitis, reflect these underlying immune and hormonal adjustments. Therefore, understanding these dynamics is essential for addressing postpartum hepatitis effectively.
Risk Factors and Prevention
Identifying key risk factors for postpartum hepatitis is essential in developing effective prevention strategies. Hormonal influences play a significant role in liver function and maternal immunity, making these critical areas of focus. During and after pregnancy, these hormonal changes can exacerbate liver issues, leading to heightened vulnerability. Enhancing maternal immunity through careful monitoring and support can mitigate risks. Furthermore, antiviral therapy plays a pivotal role, particularly for those with chronic conditions like HBV, where managing the virus becomes essential to prevent flare-ups postpartum. Additionally, addressing pregnancy complications promptly and effectively can prevent the progression to hepatitis. Overall, tailored care and preventive measures suited to individual risk profiles are crucial for protecting maternal health after childbirth.

Monitoring and Management
Effective monitoring and management of hepatitis after pregnancy are key to mitigating potential complications and ensuring maternal health. Management strategies prioritize regular clinical evaluations to monitor liver function through blood tests, particularly tracking ALT levels. Monitoring protocols include periodic assessments of immune function, recognizing the unique alterations postpartum**. Immune modulation plays a pivotal role, as the immune system recalibrates after pregnancy, potentially affecting hepatitis severity or recovery.** Therapeutic interventions might be necessary, especially in cases where hepatitis exacerbates. These interventions are tailored to individual clinical outcomes, ensuring that treatments align with the specific health needs of the postpartum patient. Such thorough management ensures better health trajectories for mothers recovering from hepatitis.
Research Insights and Future
Exploring recent research, several innovative insights and potential directions have emerged for managing and understanding postpartum hepatitis. Future research is focusing on immune modulation and hormonal influence to develop more effective treatment strategies**. Understanding the dynamics of immune recovery and the role of pregnancy-related hormones could lead to breakthroughs in maternal health care.** Researchers are particularly interested in how hormonal shifts contribute to postpartum hepatitis onset and progression, aiming to tailor interventions that address these specific changes. Additionally, studies are exploring how immune modulation could prevent or mitigate the condition, potentially leading to innovative therapeutic strategies that enhance safety and efficacy for postpartum women. This focus on targeted treatment strategies promises to improve outcomes and quality of life for affected mothers.
Conclusion
To sum up, postpartum hepatitis, linked to immune and hormonal changes after childbirth, typically resolves on its own. Regular monitoring of ALT levels and liver function is critical. Understanding the underlying mechanisms through ongoing research could lead to better management strategies. For instance, a hypothetical case of a mother showing elevated ALT levels in the 6th week postpartum, successfully monitored and managed, underscores the importance of timely intervention and tailored care in improving outcomes.
Bibliography
- Zhang L, Jiang T, Yang Y, Deng W, Lu H, Wang S, Liu R, Chang M, Wu S, Gao Y, Hao H, Shen G, Xu M, Chen X, Hu L, Yang L, Bi X, Lin Y, Lu Y, Jiang Y, Li M, Xie Y. Postpartum hepatitis and host immunity in pregnant women with chronic HBV infection. Front Immunol. 2023 Jan 4;13:1112234. doi: 10.3389/fimmu.2022.1112234. PMID: 36685527; PMCID: PMC9846060. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9846060/)
- Li L, Zou H, Xu M, Li S, Zhu Y, Zheng S, Duan Z, Chen Y. Risk factors related to postpartum hepatic inflammation in pregnant women with chronic hepatitis B. J Int Med Res. 2020 Nov;48(11):300060520966439. doi: 10.1177/0300060520966439. PMID: 33208011; PMCID: PMC7683929. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7683929/)
- Samuel D, Riordan S, Strasser S, Kurtovic J, Singh-grewel I, Koorey D. Severe autoimmune hepatitis first presenting in the early post partum period. Clinical gastroenterology and hepatology. 2004;2(7):622-624. doi:https://doi.org/10.1016/s1542-3565(04)00245-9 (https://www.cghjournal.org/article/S1542-3565(04)00245-9/fulltext)
- Izumi Y, Kaneko A, Oku K, et al. Development of liver dysfunction after delivery is possibly due to postpartum autoimmune hepatitis. A report of three cases. Journal of internal medicine. 2002;252(4):361-367. doi:https://doi.org/10.1046/j.1365-2796.2002.01047.x (https://onlinelibrary.wiley.com/doi/pdf/10.1046/j.1365-2796.2002.01047.x)
- Wang X, Song A, Lin X, et al. Clinical characteristics of hepatitis flares during pregnancy and postpartum in Chinese chronic hepatitis B virus carriers—a prospective cohort study of 417 cases. Frontiers in immunology. 2022;13. doi:https://doi.org/10.3389/fimmu.2022.1031291 (https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.1031291/full)
- CDC. Protect Your Baby for Life.; 2011. (https://www.cdc.gov/hepatitis/HBV/PDFs/HepBPerinatal-ProtectWhenPregnant.pdf)