Cholangiocarcinoma at Hepatic Hilum
Cholangiocarcinoma at Hepatic Hilum
Cholangiocarcinoma at the hepatic hilum epitomizes the intricate nature of hepatobiliary malignancies, presenting a conundrum that challenges clinicians and researchers alike. From its elusive epidemiological footprint to the complexities of staging and treatment modalities, this subset of cholangiocarcinoma demands a meticulous approach. Understanding the interplay of diagnostic nuances and therapeutic dilemmas is crucial in navigating the landscape of care for patients. As we explore the multifaceted dimensions of this disease entity, uncovering the evolving strategies and prognostic considerations becomes paramount for optimizing patient outcomes.
Epidemiology and Risk Factors
Cholangiocarcinoma, accounting for less than 2% of all human malignancies, exhibits a higher incidence in Asia and is influenced by various established risk factors. Epidemiological trends indicate a rising incidence of intrahepatic cholangiocarcinoma over the past two decades, with approximately 3,000 extrahepatic cases annually in the United States. Advanced age, male gender, cirrhosis, inflammatory bowel disease, and chronic pancreatitis are associated with hilar cholangiocarcinoma. Parasitic liver diseases, biliary tract stone disease, and primary sclerosing cholangitis (PSC) are significant risk factors, with PSC patients facing a lifetime incidence ranging from 6% to 36%.
Genetic predisposition, environmental influences, and occupational exposures also play roles in cholangiocarcinoma development. Understanding these risk factors is crucial for early detection and intervention strategies. Further risk factors analysis is essential to improve screening protocols and develop targeted preventive measures against this aggressive malignancy. Advanced research in genetic susceptibility and environmental triggers is vital for comprehensive risk assessment and personalized management strategies in individuals predisposed to cholangiocarcinoma.
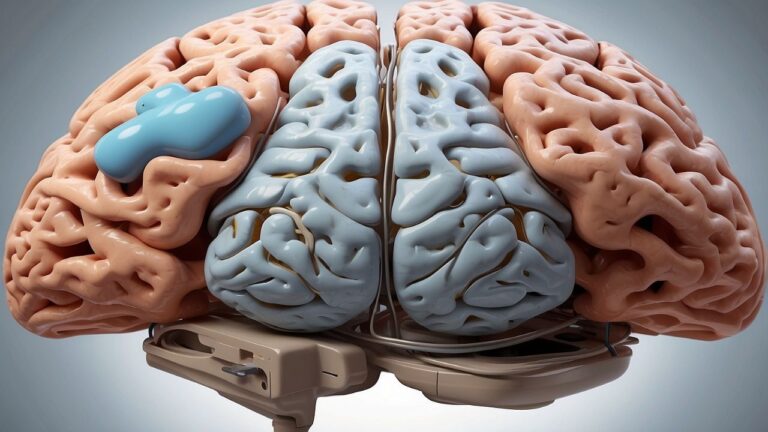
Diagnosis and Imaging
The diagnostic process for cholangiocarcinoma involves a comprehensive approach utilizing various imaging modalities to characterize the tumor and determine respectability. Radiological findings play a crucial role in identifying cholangiocarcinoma, with imaging techniques such as CT, MRI, ultrasound, ERCP, and PTC being instrumental in this process. These imaging modalities aid in tumor characterization by providing detailed information on the size, location, and extent of the lesion. They also assist in differentiating cholangiocarcinoma from other biliary tract pathologies, contributing to the differential diagnosis.
However, despite the advancements in imaging technology, diagnostic challenges persist in accurately detecting and staging cholangiocarcinoma. The subtle nature of early symptoms like jaundice and the non-specificity of imaging findings can make diagnosis challenging. Additionally, the overlap in radiological features between benign and malignant biliary lesions further complicates the diagnostic process. Therefore, a multidisciplinary approach integrating clinical presentation, imaging studies, and histopathological evaluation is essential to overcome these diagnostic hurdles and optimize patient management.

Pathological Characteristics and Staging
Analyzing the histological characteristics and implementing staging systems are essential components in the comprehensive management of cholangiocarcinoma. Tumor classification in cholangiocarcinoma includes gross classifications like papillary, nodular, and sclerosing types. Adenocarcinomas are further graded as well, moderately, or poorly differentiated, providing insights into the aggressiveness of the tumor**. Biomarker expression, such as CEA and MUC1 in hilar cholangiocarcinoma, aids in diagnosis and can influence treatment decisions.** Understanding premalignant progression is crucial as it sheds light on the evolution of cholangiocarcinoma from benign lesions to invasive cancer. Staging systems like Bismuth-Corlette and MSKCC play a vital role in categorizing the local tumor extent and assessing portal vein involvement, which is crucial for determining the optimal management approach. Furthermore, recognizing portal vein involvement is essential as it impacts the surgical planning and overall prognosis of patients with cholangiocarcinoma.
Treatment Options
Histological characteristics and staging systems play a crucial role in guiding the selection and implementation of appropriate treatment options for patients with cholangiocarcinoma. Chemotherapy poses challenges in managing unresectable tumors, with variations in outcomes based on patient functional status. Immunotherapy advancements offer a promising avenue, although further research is needed to establish their efficacy in cholangiocarcinoma. Palliative care considerations are essential for improving quality of life in advanced stages, focusing on symptom management and psychosocial support. Novel surgical techniques, such as minimally invasive procedures and orthotopic liver transplantation, show potential in selected cases, warranting ongoing investigation for broader application. Targeted therapy options, tailored to specific molecular profiles of tumors, present a personalized approach to treatment, with the aim of enhancing therapeutic efficacy and minimizing adverse effects. The multidisciplinary approach, incorporating these diverse treatment modalities, aims to optimize outcomes in patients with cholangiocarcinoma.
Prognosis and Recurrence
Considering the intricate interplay between tumor characteristics and patient outcomes, a comprehensive understanding of prognostic factors and recurrence patterns in cholangiocarcinoma is essential for informed clinical decision-making**. Survival rates following surgical resection of cholangiocarcinoma range from 10% to 40% at the five-year mark.** Despite R0 resections, recurrence risk remains high, with rates reaching 50-70%. Factors such as lymph node invasion, tumor grade, and achieving negative margins play pivotal roles in determining prognosis. Consequently, meticulous follow-up care is imperative to monitor for disease recurrence and manage potential complications. Adjuvant therapies, including chemotherapy and radiation, are often utilized to improve outcomes and reduce recurrence rates. Additionally, attention to the quality of life post-treatment is crucial, considering the physical and emotional toll of cholangiocarcinoma and its treatments. In summary, a multidisciplinary approach that includes close surveillance, appropriate adjuvant therapy, and a focus on enhancing quality of life is paramount in managing cholangiocarcinoma effectively.
Preoperative Evaluation and Staging
In the evaluation and staging of cholangiocarcinoma, a meticulous assessment of respectability criteria and tumor extent is paramount for guiding surgical management decisions and optimizing patient outcomes. Surgical planning hinges on determining respectability, which necessitates a comprehensive radiological assessment to evaluate vascular involvement and tumor extension. Respectability criteria encompass factors such as negative margins, absence of distant metastases, and specific tumor extensions, while considering the patient’s overall fitness and underlying conditions. Advanced diagnostic techniques, including CT angiography, duplex ultrasonography, and MRCP, aid in delineating tumor characteristics and predicting respectability. Staging laparoscopy plays a crucial role in detecting unresectable tumors, particularly in advanced cases, while FDG-PET scanning complements standard imaging in diagnosing and staging hilar cholangiocarcinoma. Understanding these facets through preoperative evaluation and staging is fundamental in formulating an effective surgical approach and ultimately impacting long-term patient outcomes.
Conclusion
In conclusion, cholangiocarcinoma at the hepatic hilum presents a unique challenge in diagnosis and treatment due to its rarity and complex nature. With less than 2% of all cancers being cholangiocarcinoma, the incidence of this malignancy remains low but is associated with specific risk factors. Understanding the epidemiological patterns and tailored therapeutic strategies is crucial for improving the prognosis of patients. A noteworthy statistic reveals that the 5-year survival rate for localized cholangiocarcinoma is approximately 30%.
Bibliography
- Jarnagin W, Winston C. Hilar cholangiocarcinoma: diagnosis and staging. HPB (Oxford). 2005;7(4):244-51. doi: 10.1080/13651820500372533. PMID: 18333200; PMCID: PMC2043098. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2043098/)
- Soares KC, Kamel I, Cosgrove DP, Herman JM, Pawlik TM. Hilar cholangiocarcinoma: diagnosis, treatment options, and management. Hepatobiliary Surg Nutr. 2014 Feb;3(1):18-34. doi: 10.3978/j.issn.2304-3881.2014.02.05. PMID: 24696835; PMCID: PMC3955000. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3955000/)
- Soares KC, Kamel I, Cosgrove DP, Herman JM, Pawlik TM. Hilar cholangiocarcinoma: diagnosis, treatment options, and management. PubMed. 2014;3(1):18-34. doi: https://doi.org/10.3978/j.issn.2304-3881.2014.02.05 (https://hbsn.amegroups.org/article/view/3374/html)
- Hilar cholangiocarcinoma – Overview – Mayo Clinic. Mayoclinic.org. Published 2023. Accessed February 26, 2024. (https://www.mayoclinic.org/diseases-conditions/hilar-cholangiocarcinoma/cdc-20354548)